MRI Audit May 2017
27/09/17 16:35 Filed in: Events
In May I attended the Kuring-Gai District Medical Association conference at Uluru and presented my personal experience of prostate MRI. Over the four year period to February 2017 300 prostate Mri studies were performed, all but a few at the Sydney Adventist Hospital. These are technically complex studies which need to be performed by expert technicians and accurately reported by experienced radiologists. If normal a PI-RADS grading score of 1 is allocated. Abnormal findings are graded from 2 to 5: 2 indicates a minor abnormality, 3 possibly benign, possibly cancer, 4 moderately suspicious for significant cancer, and 5 almost certainly significant cancer.
Prostate biopsies are recommended for PI-RADS 3,4 and 5 lesions but not routinely for 1 and 2 lesions. I was interested in the outcome of biopsies in the various categories. In particular whether it is safe to omit biopsies in category 1 and 2 lesions, and how likely it is to diagnose significant cancer in categories 3,4 and 5.
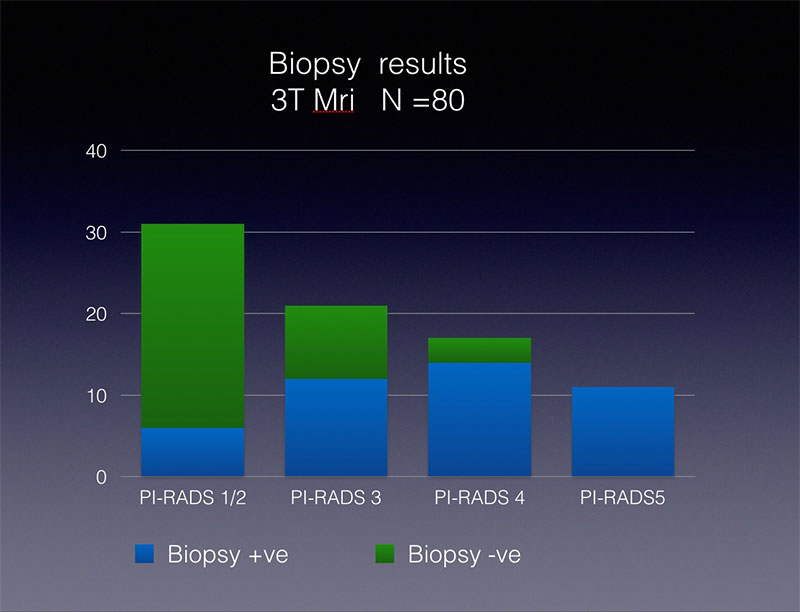
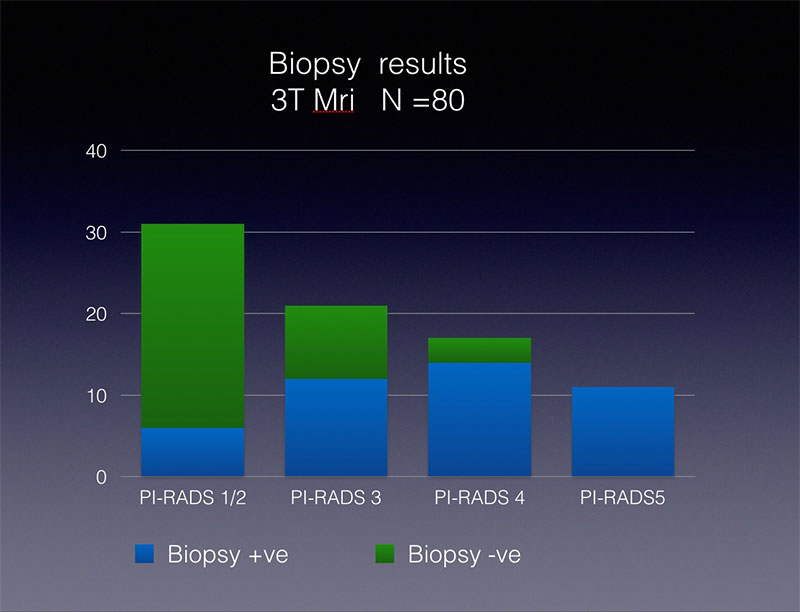
The results were more reliable for studies performed on the new 3T scanner (installed in February 2015) so I presented only this data. Eighty patients with 3T scans proceeded to biopsy with the following results:
The clinical implications are:
Firstly, a negative Mri does not rule out significant cancer and biopsies should be performed if clinically indicated. If not patients need careful followup.
Secondly the risk of significant cancer in PI-RADS category 3 in this series was higher than expected. Although the numbers are small they support the recommendation that all patients with PI-RADS 3 as well as PI-RADS 4 and 5 should be biopsied.
Thirdly, a further finding was that significant cancer would have been missed in 13% if biopsies were only taken from the lesions seen on MRI. Therefore targeted and systematic biopsies should be performed. Significant cancer was found in 55% of systematic biopsies. Knowing the full extent of the cancer helps to plan treatment.
Prostate biopsies are recommended for PI-RADS 3,4 and 5 lesions but not routinely for 1 and 2 lesions. I was interested in the outcome of biopsies in the various categories. In particular whether it is safe to omit biopsies in category 1 and 2 lesions, and how likely it is to diagnose significant cancer in categories 3,4 and 5.
The results were more reliable for studies performed on the new 3T scanner (installed in February 2015) so I presented only this data. Eighty patients with 3T scans proceeded to biopsy with the following results:
- PI-RADS 1 and 2 (low risk)
15% had significant cancer - PI-RADS 3 (borderline risk)
60% had significant cancer and of these two thirds had very aggressive cancer - PI-RADS 4 (cancer likely)
85% had significant cancer. Three patients had negative biopsies and will need close surveillance with a view to repeat biopsies. - PI-RADS 5 (cancer almost certain) 100% had significant cancer.
The clinical implications are:
Firstly, a negative Mri does not rule out significant cancer and biopsies should be performed if clinically indicated. If not patients need careful followup.
Secondly the risk of significant cancer in PI-RADS category 3 in this series was higher than expected. Although the numbers are small they support the recommendation that all patients with PI-RADS 3 as well as PI-RADS 4 and 5 should be biopsied.
Thirdly, a further finding was that significant cancer would have been missed in 13% if biopsies were only taken from the lesions seen on MRI. Therefore targeted and systematic biopsies should be performed. Significant cancer was found in 55% of systematic biopsies. Knowing the full extent of the cancer helps to plan treatment.